Human Coronary Artery Endothelial Cells: Plaque: HCAEC-q
Description
Human Coronary Artery Endothelial Cells (HCAEC) from Cell Applications, Inc. provide an excellent model system to study all aspects of cardiovascular function and disease, and they have been utilized in dozens of research publications, for example to:
- Understand the mechanism of the anti-inflammatory properties of HDL, and demonstrate for the first time that mature miRNA can control gene expression in a cell where it is neither transcribed nor processed
- Study mechanisms of angiogenesis, as well as oxidative stress and inflammation related pathways in endothelia, including gender and race specific differences in patients with peripheral artery disease
- Elucidate molecular mechanisms of various cardiovascular risk factors, including those associated with diabetes
- Understand the mode of action and cardiovascular protection effects of various natural compounds, vitamins and drug candidates
- Develop and evaluate scaffolds and hydrogels for cardiac tissue engineering, and new treatment strategies to prevent stent restenosis
- Compare effects of BMP-4 on HCAEC and Human Pulmonary Artery Endothelial Cells (HPAEC, also from Cell Applications, Inc.)
- Show that only in HCAEC BMP-4 treatment induced ROS, activated NF-kB, ICAM-1 and increased monocyte adhesiveness, explaining why its upregulation leads to atherosclerosis and hypertension in the systemic, but not pulmonary circulation
Additionally, HCAEC, along with human aortic (HAOEC), carotid artery (HCtAEC), subclavian artery (HScAEC) and brachiocephalic artery (HBcAEC), all provided by Cell Applications, Inc., have been used to demonstrate that not only blood vessels from different tissues are highly heterogeneous, they also interact differently with leukocytes during the inflammation response. The authors further showed that differential N-glycosylation of commonly expressed vascular adhesion molecules may be responsible for this heterogeneity, as well as for modulation of signaling under resting and activated inflammatory conditions. This also explains why specific vascular beds may be more or less susceptible to particular diseases or stimuli. Importantly, if cells from different sources were used, these results could not be convincingly validated due to a number of uncontrolled variables, such as age, race, genetic variability or life style choices of the donors. To eliminate the donor-to-donor variability, the scientists took advantage of the great variety of primary cells offered by Cell Applications, including the option of ordering a panel of endothelial cells obtained from different vascular beds of the same donor!
Because of the complex heterogeneity that exists not only between different donors, but even between different vascular beds in the same individual, it would be prudent to confirm any new findings on primary cell lots coming from several different origins.
Details
| Tissue | Normal healthy human coronary artery | |
|---|---|---|
| QC | No bacteria, yeast, fungi, mycoplasma, virus | |
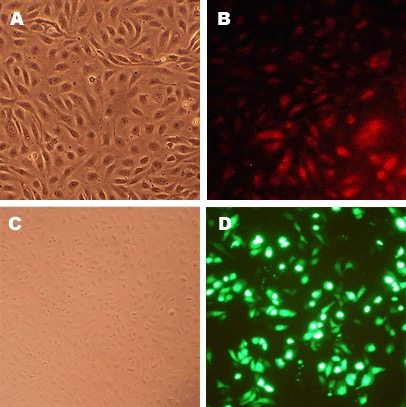
| Character | Factor VIII-related Ag, DiI-Ac-LDL uptake | |
| Bioassay | Attach, spread, proliferate in Growth Med | |
| Cryovial | 500,000 HCAEC-q (2nd passage) frozen in Basal Medium w/ 10% FBS, 10% DMSO | |
| Kit | Cryovial frozen HCAEC-q (300q-05a), Growth Med (212-500), Subculture Rgnt Kit (090K) | |
| Proliferating | Shipped in Gr Med, 3rd psg (flasks or plates) | |
| Doublings | At least 15 | |
| Applications | Laboratory research use only (RUO). Not for human, clinical, diagnostic or veterinary use. |
Resources
FAQs
Need More Help?
Visit our comprehensive FAQ page for detailed answers to common questions.
Need More Help?
Visit our comprehensive FAQ page for detailed answers to common questions.
Primary Cell FAQs